Audit Processing in Healthcare: How to Streamline Medical Record Requests
Audit Processing in Healthcare Audit season is here, and for many healthcare providers, that means...
In recent years, many healthcare providers have transitioned from manual, outdated systems to streamlined e-billing processes for group health claims. Now, healthcare providers benefiting from these efficient e-billing solutions are calling for similar advancements in the P&C sector. Specifically, they seek 270/271 eligibility processing to align with their existing group health workflows. However, the complexity and extensive data requirements of workers’ compensation and auto casualty claims do not fit neatly into traditional 270/271 Eligibility ANSI file formats, posing a challenge for P&C claims processing.
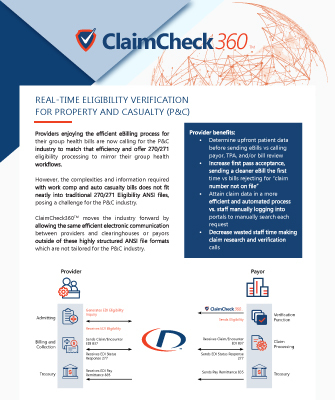
With ClaimCheck360™, providers can benefit from a more simplified claim process. The benefits include:

