Payor clients of Medlogix (insurance companies, employer groups, TPAs and more) that accept or route transactions from submitters to Medlogix for adjudication
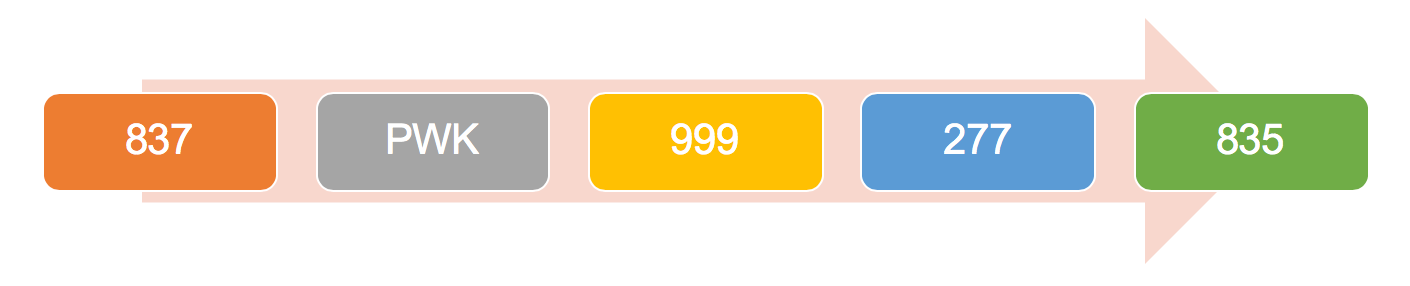
Medlogix issues unique Payor IDs to each of their client receivers to help control the flow of EDI even when things change. If another clearinghouse or billing vendor has assigned a proprietary Payor ID to our client’s route, our designated EDI clearinghouse (Data Dimensions, a/k/a AccidentEDI) can accept either identifier and route the billing correctly.
Yes….our designated clearinghouse, Data Dimensions, is the largest P&C clearinghouse in the country. They are able to accept EDI directly from submitters or indirectly through a submitter’s eBilling trading partner or clearinghouse. To learn more about submitter options please reach out to us.
Yes…Medlogix can aggregate prospective transactions from submitters as well as handle the exchange of retrospective billing from customers and third-party vendors.
All of our clients are fully compliant with all state mandate requirements. We offer an array of flexible eBilling submission methods that are sure to meet the needs of our client’s submitters.
Medlogix institutes a proven Provider Outreach & Education program with its designated EDI vendor partner, Data Dimensions, that strategically and tactically targets paper submitters and drives messaging to ensure EDI options are presented. This program was built with over 20+ years of eBilling experience and has proven to dramatically increase the EDI volume to a receiver client.
Medlogix clients will soon be able to extend numerous electronic payment modalities to submitters, including (but not limited to) ACH, Digital Checks, Virtual Cards and physical Checks. Customers will also have a robust “opt-out” solution that will ensure submitter satisfaction with selecting the option that is right for their office.
If using clearinghouse, bill level notifications will come from clearinghouse first, then Payor or Bill Review company